I first encountered science seriously as a health consumer advocate, a very long time ago. And I thought of medical and health research as a search for answers. Scientists were problem-solvers, using rigorous testing to sort out the wheat of reliable answers from the chaff of the false leads.
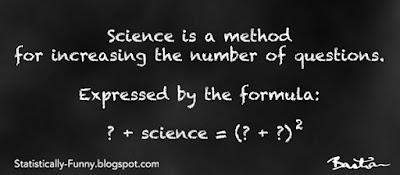
But over time, as I watched the research pile up exponentially, the number of questions was zooming up even faster.
We find out treatment A works. Who – and what – else could it work for? Can you have half the dose and still get just as much benefit? Does double the dose do more good than harm? Will it work even better if you combine it with treatment B? Combine it with treatment C? Combine it with B and C? Is it better than old treatment Q? Will work it in gel form? In spray? . . .
Turns out scientific studies are, in fact, a great way to generate more questions. Answers, on the other hand, are often elusive.
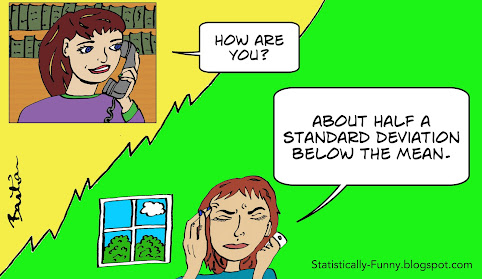
So whose questions does science work with? For most of science’s history, the work has been dominated by one gender and one race, from just a few countries. The barriers to scholars from the Global South and access to, and recognition of, their work internationally remain shockingly high. On top of that, scientists typically worked at arm’s length from the people affected by the problems they were trying to solve. The result was often a very narrow set of questions.
Consider the experience of clinical researchers in rheumatology. It wasn’t until after the field embraced consumer participation that fatigue, sleep, and disease flares were seen as important outcomes to measure. And the process changed their research culture, too.
Diversity in science is critical, too, to bring a variety of perspectives to the question-asking table. That includes diversity of disciplines in scientific teams. Working across disciplines doesn’t just bring different points of views into the process. It can be essential for scientific quality. Poor scientific methods that have been rejected in some disciplines, persist in other parts of academia. Interdisciplinary science might be able to spread superior scientific methods into fields with weaker science.
If questions are so important to how our knowledge grows – and they are – then the issue of who gets to ask those questions is a fundamental concern. It can have a profound impact on what questions get addressed at all, and what is seen.
(This post is based on a 2019 post at Absolutely Maybe, drawing on the point on interdisciplinary science elaborated on in a 2022 post at Living With Evidence.)